Skin damage
Occupational skin damage and diseases present great challenges for practical and academic occupational medicine. In the Ordinance on Occupational Diseases, work-related skin damage is listed as an occupational disease under Number 5101. In this section, occupational diseases of the skin (BK5101) are defined as “severe or repeated skin changes that have forced the patient to refrain from all activities that were or may be the cause for the occurrence, exacerbation, or recurrence of the disease”. Although confirmed cases have decreased slightly in recent years, these forms of skin diseases—at a proportion of 28% of all occupational diseases—are the most commonly reported work-related illness in Germany.
| BK 5101 (skin diseases) | 2015 | 2016 | 2017 |
| suspected cases | 23.786 | 22.574 | 21.063 |
| confirmed cases | 20.457 | 19.641 | 18.422 |
| recognised cases | 578 | 533 | 515 |
according to the DGUV
hhttps://www.dguv.de/en/facts-figures/ods/notifications-od/index.jsp
https://www.dguv.de/en/facts-figures/ods/recognized-od/index.jsp
Recommendations on the assessment of skin diseases have been summarised in the „Bamberger Merkblatt Teil I: Begutachtungsempfehlungen für die Begutachtung von Hauterkrankungen“.
Occupational skin diseases primarily affect the hands, as this is the part of the body that comes into contact with hazardous substances most frequently. Irritant or toxic and/or allergic hand eczema are the most commonly reported types of work-related hand eczema. In contrast, the proportion of other occupational dermatoses (see Figure 3) is quite small. Due to the high prevalence or incidence of work-related skin damage, preventive measures for the protection of the skin are a high priority. This work generally requires cooperation with (occupational) dermatologists, either directly or via teledermatology.
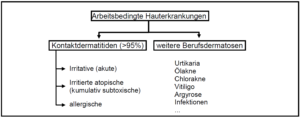
Figure 3: Occupational skin diseases (adapted from Drexler 2007, Kompetenzzentrum Arbeitsmedizinische Dermatotoxikologie)
Skin damage may lead to an inhibition in the barrier function of the skin. The physiological homeostasis of the skin may also be affected. Regulated skin homeostasis is, however, an important factor in many dermal physiological, immunological, and biochemical processes. Certain physical (sun, heat…), chemical (acids, bases…), or biological (allergens such as nickel, chromium…) factors may damage the skin to such an extent that it inhibits the skin’s ability to function. The first symptoms of such damage are often redness and swelling in the affected area.
Irritative or toxic contact dermatitis
Irritative, acute skin damage is generally characterised by accidental exposure, whereby the skin is corroded by contact with hazardous substances such as acids or bases.
Frequent, consecutive contact over a short period of time to a (primarily) non-corrosive noxious substance (e.g. increased hygiene measures such as hand-washing) can lead to irritative, cumulative, and subtoxic skin damage. Occurrence of this form of skin eczema can be facilitated by predisposition to atopy (atopic diathesis).
- The skin barrier is inhibited in its function,
- reddening of the skin, itchiness, flaking, keratinisation disorders of the skin
- generally limited to the area of contact
The skin damage acquired from irritant, cumulative, and subtoxic contact eczema facilitates the development of an (additional) allergic contact eczema (bi- or multiphasic eczema).
Irritant contact eczemas are the more frequently occurring form of work-related eczemas, but are generally more mild than allergic eczemas.
Allergic contact eczema
In cases of allergic contact eczema, T cells (T lymphocytes) are sensitised by contact with an allergen (direct contact or via ambient air). After renewed contact with the allergen in question, a type-IV allergic reaction takes place after 24 to 48 hours (delayed or late onset), specifically allergic contact eczema. This condition first presents with an itchy redness at the contact site as well as the formation of pustules and oedematous swelling. Allergic contact eczema frequently expands beyond the actual area of contact with the allergen.
Allergic contact eczemas are the less frequently occurring form of work-related eczemas, and are generally more severe than irritant eczemas; for this reason, it is more often necessary for workers to leave their profession if a case of allergic contact eczema arises.
Prevention
The preventive measures for occupational dermatology are categorised as follows:
| primary prevention | for healthy workers – workplace prevention |
| secondary prevention | upon first onset of symptoms – avoid chronification – avoid sensitisation / allergic contact eczema |
| ttertiary prevention | in cases of a manifested skin disease – pursue curative care / avoid exacerbation |
Preventive measures:
– Minimisation of skin exposure (organisational and technical measures)
- Classes on skin-protection measures
- Change of position or of career
– individual skin protection (gloves, skin-protection preparations)
- Use of skin-protection preparations both pre- and post-exposure
– Skin-protection salves (barrier creams) inhibit or reduce the effects of the substance(s) on the skin
– Skin-cleansing agents rid the skin of the substance(s)
– Skin care should support skin regeneration/repair and support CAVE: gloves
– Occlusion
– Sensitisation (e.g. latex gloves, immunoglobulin-assisted Type I; or allergic reactions from additives Type IV) CAVE: skin-protection salves
– may facilitate the systemic absorption of substances
HEROS (hand eczema score for occupational screenings)
The HEROS (hand eczema score for occupational screenings) is a qualitative, validated score for the evaluation of the skin condition of the hands; the spread and intensity of all skin changes typical for hand eczema can be documented using this tool. This objective score, which was developed for preventive care in the field of occupational medicine, can reliably measure minimal skin changes for persons with mostly healthy skin or can examine the efficacy of preventive measures.
With HEROS, all skin changes typical for hand eczema can be measured, including erythema, papules, pustules, erosion, flaking / hyperkeratosis, lichenification, fissures, crustiness / excoriations, and xerosis. To this end, the surface of the hand is divided into 54 areas of about equal measure whereby, wherever possible, anatomical structures are followed. The intensity of the given skin change is indicated on a scale of 0 (no change) to 3 (severe change), with the exception of lichenification, for which intensity is measured on a scale of 0 to 2. For the measurement of palm erythema, the entire inner surface of the hand is considered as a single area, so that frequently occurring vascular dilations are not evaluated or overestimated as specific skin changes. The same process holds true for the lichenification of the inner surface of the hand. For the evaluation of xerosis, one hand (dorsal and palmar) is considered to be one area (value for one hand corresponds to a maximum 3 points in the score). After examination of both hands, the points for individual skin changes are summed into a HEROS value.
There was excellent consistency in the investigation of intra- and interobserver variability, with scores in the range of others which were validated in patients with a manifest case of hand eczema. HEROS is therefore a validated, quantitative skin score with which the skin condition of the hands can be quickly and objectively documented.
The HEROS evaluation sheet can be downloaded here.
References
Weistenhöfer W, Baumeister T, Drexler H, Kütting B. How to quantify skin impairment in primary and secondary prevention? HEROS: a proposal of a hand eczema score for occupational screenings. Br J Dermatol 2011; 164 (4): 807-813 https://onlinelibrary.wiley.com/doi/full/10.1111/j.1365-2133.2010.10181.x
Weistenhöfer W, Baumeister T, Drexler H, Kütting B. An overview of skin scores used for quantifying hand eczema: a critical update according to the criteria of evidence-based medicine. Br J Dermatol 2010; 162 (2): 239-250. Review https://onlinelibrary.wiley.com/doi/full/10.1111/j.1365-2133.2009.09463.x
Contact person: PD Dr. med. Wobbeke Weistenhöfer
„Malignant skin tumours induced by UV radiation – Development and evaluation of criteria relevant to insurance law for distinguishing occupational from non-occupational causation; Part 2: Case-control study on the relationship between work-related and non-work-related exposure to UV radiation and skin cancer in A) squamous cell carcinoma and B) basal cell carcinoma (FB 181)“
– multicentre study –
The research project was financed by the DGUV (FB 181).
Natural, solar UV radiation is an important risk factor for the occurrence of cutaneous squamous cell carcinoma (Plattenepithelkarzinomen, PEK) and basal cell carcinoma (Basalzellkarzinomen, BZK), whereby the dose-response relationship between UV exposure and the risk of contracting PEK and BZK as well as the relevance of occupational UV exposure for the occurrence of BZK has not yet been thoroughly researched.
A population-based, multicentric, case-control study was conducted with two case groups (incidental spontaneous PEK; incidental spontaneous BZK) as well as a control group; a total of 626 persons with PEK/third-degree actinic keratosis or Bowen’s disease, 739 people with BZK, and 996 controls were recruited and examined. Occupational and non-occupational UV exposure was determined using the instruments developed in the FB 170 research project for the quantification of light damage. Known risk factors–such as positive family history, skin type, immunosuppression, age, and gender–were taken into account when analysing the relationship between UV exposure and disease risk.
It could be shown that individuals with high total-exposure levels to UV radiation, compared to persons with average total-exposure levels, are at a significantly increased risk of contracting squamous cell carcinoma of the skin (Odds Ratio (OR) = 1.7; 95% confidence interval 1.0–2.8). A statistically significant correlation could not be established for persons with basal cell carcinoma, but a clear trend was evident (OR = 1.5; 95% confidence interval 0.9–2.2).
In contrast, it could be proven for both PEK and BZK that persons with high levels of occupational exposure to natural UV radiation exhibit a considerably increased disease risk. Compared to persons with an average level of occupational exposure, persons with high levels of occupational UV radiation were more than twice as likely to develop a PEK (OR = 2.4; 95% confidence interval 1.5–4.0) and are about twice as likely to develop a BZK (OR = 2.0; 95% confidence interval 1.2–3.2) compared to persons with an average level of occupational exposure to natural UV radiation. Career groups with especially high risk of contracting both tumor entities include agricultural work, animal and plant husbandry, outdoor construction, and locksmiths/installers/pipe fitters (with outdoor employment).
Another significant finding compared to previous studies is the demonstration of positive dose-response relationships between cumulative total exposure to natural UV radiation and the risk of developing squamous cell carcinoma or basal cell carcinoma of the skin. These positive dose-response relationships are not independent of the origin (occupational or non-occupational) of UV exposure for both PEK and BZK. For the non-occupational natural UV exposure determined in the study, no clear dose-response relationship could be shown with disease risk. In contrast, doubling doses for both squamous cell carcinoma (6,348 SED) and basal cell carcinoma (7,945 SED) could be determined for the dose-response relationships for occupational UV exposure. A possible modification by skin type was not investigated and remains subject to further analysis. For the type of UV exposure (natural/artificial), an association was shown for both PEK and BZK in such a way that visiting tanning salons increases the risk of the disease. The analyses also showed that the instruments developed in the FB 170 research project for quantifying light damage and individual occupational and non-occupational UV exposure also provide to be sufficiently valid, reliable, and practicable in the field study when used by examiners not involved in the development of the instruments. However, they require the medical staff to undergo training.
The study data collected is characterised both by its representativeness with regard to the selected parameters and by the high quality ensured by monitoring, electronic data collection, and careful plausibility checks.
With the completion of the FB 181 research project, results are now available which provide significant new starting points for the discussion of the role of occupational and non-occupational UV exposure in the development of non-melanocytic skin cancer.
References
Bauer A, Haufe E, Heinrich L, Seidler A, Schulze HJ, Elsner P, Drexler H, Letzel S, John SM, Fartasch M, Brüning T, Dugas-Breit S, Gina M, Weistenhöfer W, Bachmann K, Bruhn I, Lang BM, Brans R, Allam JP, Grobe W, Westerhausen S, Knuschke P, Wittlich M, Diepgen TL, Schmitt J; FB181 study group. Basal cell carcinoma risk and solar UV exposure in occupationally relevant anatomic sites: do histological subtype, tumor localization and Fitzpatrick phototype play a role? A population-based case-control study. J Occup Med Toxicol 2020; 15: 28. doi: 10.1186/s12995-020-00279-8. eCollection 2020. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7488106/pdf/12995_2020_Article_279.pdf
Schmitt J, Haufe E, Trautmann F, Schulze HJ, Elsner P, Drexler H, Bauer A, Letzel S, John SM, Fartasch M, Brüning T, Seidler A, Dugas-Breit S, Gina M, Weistenhöfer W, Bachmann K, Bruhn I, Lang BM, Bonness S, Allam JP, Grobe W, Stange T, Westerhausen S, Knuschke P, Wittlich M, Diepgen TL; FB 181 Study Group. Occupational UV-exposure is a Major Risk Factor for Basal Cell Carcinoma: Results of the Population-Based Case-Control Study FB-181. J Occup Environ Med 2018; 60: 36-43 https://journals.lww.com/joem/fulltext/2018/01000/Occupational_UV_Exposure_is_a_Major_Risk_Factor.7.aspx
Schmitt J, Haufe E, Trautmann F, Schulze HJ, Elsner P, Drexler H, Bauer A, Letzel S, John SM, Fartasch M, Brüning T, Seidler A, Dugas-Breit S, Gina M, Weistenhöfer W, Bachmann K, Bruhn I, Lang BM, Bonness S, Allam JP, Grobe W, Stange T, Westerhausen S, Knuschke P, Wittlich M, Diepgen TL; FB 181 Study Group, Bieber T, Brans R, Brecht B, Grabbe S, Küster D, Ruppert L, Stephan V, Thielitz A, Zimmermann E. Is ultraviolet exposure acquired at work the most important risk factor for cutaneous squamous cell carcinoma? Results of the population-based case-control study FB-181. Br J Dermatol 2018; 178: 462–472 https://onlinelibrary.wiley.com/doi/full/10.1111/bjd.15906
Contact person: Dr. med. Julia Hiller, PD Dr. med. Wobbeke Weistenhöfer
Syncarcinogenic effects of UV radiation (BK 5103) and polycyclic aromatic hydrocarbons (BK 5102) in the emergence of squamous cell carcinomas?
– systematic review
In this project, a systematic literature search of German and English publications on the question of the syncarcinogenic effect of UV radiation and polycyclic aromatic hydrocarbons (PAHs) in the PubMed, Web of Science, and EMBASE databases (if necessary, considering German occupational dermatology studies not included there) will examine whether there is scientific evidence for or against a syncarcinogenic effect of UV radiation and PAHs in the development of squamous cell carcinomas. If there is scientific evidence for a syncarcinogenic effect, it should be examined whether exposure ratios can be defined for certain groups of people. A possible syncarcinogenic effect would affect a large proportion of outdoor workers (bricklayers, civil engineers, farmers) who were exposed not only to UV radiation but also to substances classified under BK 5102 (tar, bitumen, carbolineum, etc.).
Taking the PRISMA statement into account, the following questions were addressed in a systematic review:
(i) Is there reliable data or evidence for a syncarcinogenic effect of PAHs and UV radiation?
(ii) Is there scientific proof or indications that would refute this syncarcinogenesis?
(iii) If yes, can exposure ratios be defined for certain demographic groups?
In an additional mechanistic study, different skin models (e.g. keratinocytes, ex-vivo skin) are exposed to B[a]P and UV radiation in a dose-dependent manner. The carcinogenic potential is evaluated by test batteries (e.g. micronucleus, comet assay, p53). In addition, mechanisms (e.g. oxidative homeostasis, energy metabolism) as well as uptake, metabolism, and localisation of B[a]P are investigated. Benchmark calculations will be used to define thresholds that mark the transition to an adverse state.
This project was financed by the DGUV (FB 275).
Contact person: Dr. med. Julia Hiller, PD Dr. med. Wobbeke Weistenhöfer, Regina Lutz